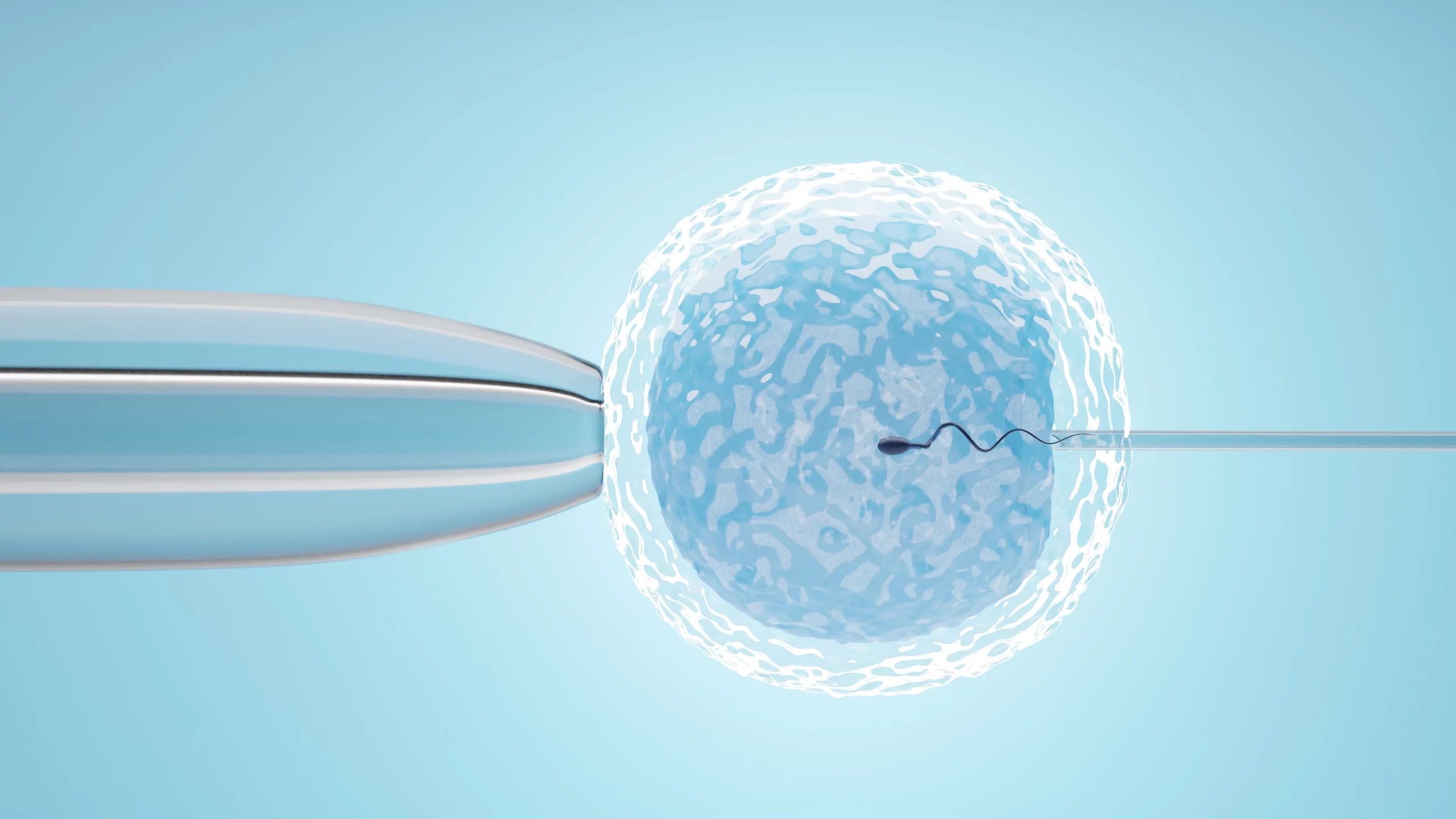
While many may think that going for fertility treatment means undergoing IVF, that is not the case. Fertility treatment options in Singapore can be categorized briefly into medical treatment, surgical treatment and Assisted Reproductive Techniques (ART), which includes in-vitro fertilization (IVF) and intra-uterine insemination (IUI).
There are also different treatments available for male and female infertility. For male infertility, the fertility specialists can provide medications to improve sperm quality and count. Improving the sperms can help to increase the chances of conceiving without IVF sometimes, and even if IVF is required, better quality sperms can help to improve the success rates. The rest of the fertility treatment options described here are mainly used to address female infertility issues.