The topic of pelvic floor dysfunction is one many women prefer to brush under the carpet as they may find its symptoms frustrating and embarrassing. In reality, pelvic floor disorders are common, affecting 1 in 4 women between the ages of 30 to 70 globally.
What Exactly is Pelvic Floor Dysfunction?
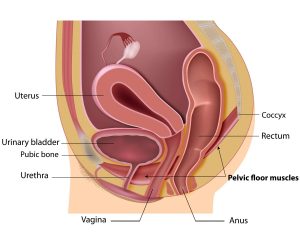
Pelvic floor dysfunction is caused by weakened pelvic floor muscles and/or tears in the connective tissues that hold the pelvic organs (bladder, uterus, rectum) in position.
They may be strained by factors such childbirth, ageing, obesity or abdominal weight gain, chronic constipation, or physically strenuous exercise.
When the connective tissue is no longer able to hold the uterus in place and they drop into the vagina, this is known as uterine prolapse and will require treatment.
There are several symptoms of pelvic floor disorders, including:
- Urinary Incontinence
Loss of bladder control is a common although often embarrassing problem faced by many women of all ages. Women with this condition may experience some urine leakage when coughing, sneezing or lifting heavy items. They may also experience sudden and intense urges to urinate followed by uncontrolled loss of urine. - Bowel Incontinence or difficulty having regular bowel movements
- Pain during sex
- Experiencing organs bulging from the vagina or a heavy feeling in the pelvic area
- Lower back pain
How is Pelvic Floor Dysfunction treated?
Treatment and management of pelvic floor dysfunction depends on the severity of the condition.
-
Pelvic Floor Exercises
Physical therapy is helpful for milder cases or after childbirth. Symptoms such as incontinence and sexual difficulty can be managed through doing certain pelvic floor exercises regularly that help strengthen the core muscles.
-
Pessaries
This is a non-surgical treatment for pelvic floor disorders. A pessary is a removeable device which is placed in the vagina to support the prolapsed tissue and hold the uterus in place.
-
Surgery
If the prolapse is substantial or severe, your gynaecologist may suggest pelvic floor surgery to reconstruct the pelvic anatomy. This may be done via open or laparoscopic methods. In some cases, a hysterectomy (removal of the uterus) may be required.
For more information on the diagnosis and treatment of pelvic floor disorders, make an appointment with our gynaecologists.
