Menstruation occurs at the end of every cycle when the inner lining of the womb breaks down and is expelled as menstrual blood. These inner lining cells are unique and are not meant to be found anywhere else in the body except in the womb’s inner lining (called the “endometrium”). In about 10% of women however, some of these cells are found in the body outside the womb and this is a condition known as Endometriosis.
The most common explanation for the above occurrence is that of retrograde menstruation – this means that some part of menstrual flow goes backwards into the pelvis through the fallopian tubes.
The Common Face of Endometriosis
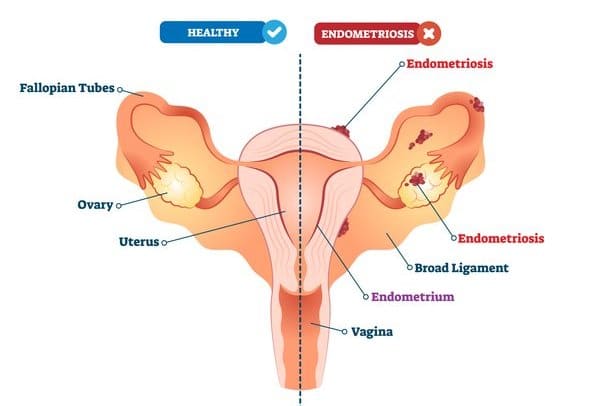
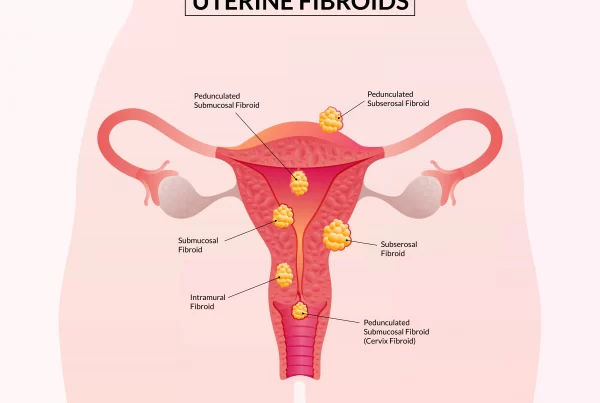
The most common sites for endometriosis implantation are the ovaries and uterosacral ligaments. Since the pelvis has important structures such as the bladder, uterus and fallopian tubes, ovaries, rectum, ureter and other important ligaments and nerves, the backflow of menstrual blood into the pelvis also means that endometriosis can affect such organs.
What are the typical symptoms of endometriosis?
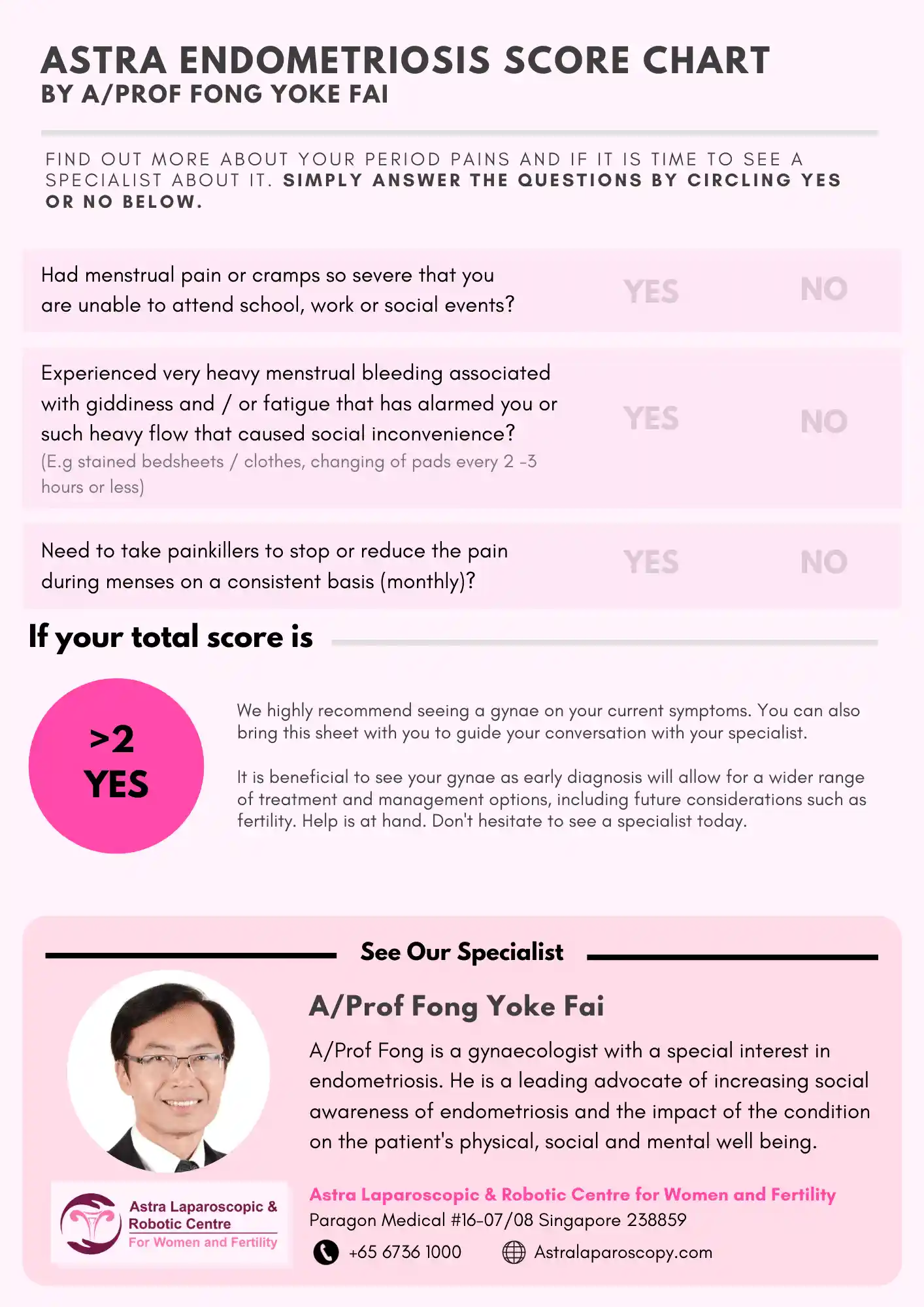
The typical symptoms of endometriosis include:
- Menstrual pain; some women have such bad pains they cannot go to school or work, or must take strong painkillers
- Heavy menses (endometriosis of the uterus)
- Rectal pain or increased sensation of wanting to pass motion during menses (when the endometriosis irritates the rectum or invades into the rectum in severe cases
- Bloated abdomen because of large endometriotic or “chocolate” cysts of the ovary.
- Backaches (endometriosis of the uterus and / or the pelvic ligaments) or shooting pain down the leg (nerve / ligament entrapment)
- Fertility issues, because the endometriosis has affected the fallopian tubes and ovaries
- Painful sex, because of the scarring and fibrosis (hardening) of the surrounding tissues that also causes nerve irritation.
What increases the chances of endometriosis happening?
The most common risk factors are nulliparity (i.e. not having given birth before), genetic predisposition and mechanical obstruction to normal menstrual flow (usually congenital). Typically, younger women are affected (from late teens to early 30s).
Can I do anything to reduce my risk of endometriosis?
The best advice I can give is: early identification and treatment to prevent progression of endometriosis. As endometriosis is related to the onset of menstruation, which is a natural event occurring at puberty, it is not possible to change that. Lifestyle factors such as diet, weight, exercise or lack of it, use of tampons etc have not been scientifically shown to alter the risk of endometriosis too. While having a pregnancy early in life helps, that is certainly a very difficult factor to control!
One of the screening tools for endometriosis would be the assessment of the impact of menses on daily activities (see diagram below).
The Face of Endometriosis that’s Less Seen
Endometriosis can sometimes affect structures and organs that are remote or far away from the pelvis. For example, the diaphragm (muscular structure that separates the chest from the abdomen) can have endometriosis. The umbilicus or the abdominal layer can also be affected by endometriosis. Sometimes the vulva (external skin overlying the outer vagina) can also have endometriosis. Other rarer occurrences are in the lungs, in joints such as the knee, and also in the eyes.
Some of these cases are related to life events such as childbirth; others may be carried in the blood or lymphatics to distant sites where they implant.
The less common symptoms of endometriosis that some may experience:
- Frequent and painful urination during menses in the case of bladder endometriosis
- Blood in the stools during menses in the case of rectal endometriosis
- Kidney swelling when endometriosis causes constriction of the ureters (long tubular structures that bring urine from the kidney to the bladder)
- Painful sex because of vaginal endometriosis or the scarring and fibrosis that has occurred in the pelvis
- Shoulder aches or a collapsed lung (pneumothorax), and even coughing out blood during menses when endometriosis affects the diaphragm
When Does A Gynaecologist Suspect Endometriosis?
 With such a wide range of symptoms, it is not uncommon for patients and even doctors to be confused about their condition. For example, urinary symptoms may be mistaken as a bladder infection, abdominal bloatedness may be diagnosed as irritable bowel while someone with backache might see a back specialist. Many studies have shown a delay in diagnosis from onset of symptoms, some for as long as 7 years!
With such a wide range of symptoms, it is not uncommon for patients and even doctors to be confused about their condition. For example, urinary symptoms may be mistaken as a bladder infection, abdominal bloatedness may be diagnosed as irritable bowel while someone with backache might see a back specialist. Many studies have shown a delay in diagnosis from onset of symptoms, some for as long as 7 years!
A Detailed Assessment by the Endometriosis Specialists
During a consultation, the Endometriosis Specialist will often take a very detailed menstrual history and go in-depth with regard to the pain symptoms. For example:
- When did the symptoms start? Has the intensity or severity been increasing over the years? (Pain often starts in the teenage years with gradual escalation through the years.)
- Where are the symptoms affecting you? (Nerve and organ-specific symptoms are also very important.)
A thorough physical and pelvic examination is also vital to pick out disease in the pelvis.
A Key Advancement in Diagnosis and Treatment – Endometriosis Imaging
How does one know the extent of endometriosis involvement and why is it important to “map” the disease as thoroughly as possible?
In 2016, the International Deep Endometriosis Analysis group published a consensus opinion on sonographic features of the different types of endometriosis. An exciting advancement in the management of endometriosis is the use of transvaginal ultrasound for endometriosis mapping.

With good ultrasound expertise, it becomes possible to screen for adenomyosis (endometriosis of the uterus) and key structures in the pelvis such as the bladder, ureter, ovaries and fallopian tubes, ligaments (which contain nerves), the rectum and sigmoid colon and also important anatomical spaces in the pelvis.
How Accurate Imaging Impacts Treatment Outcomes
Only by knowing the type and extent of the endometriosis can the doctor enable an individualized treatment plan for the patient. Inadequate mapping will lead to underestimation and under-diagnosis of the disease, which in turn leads to under-treatment as a result of insufficient preparation.
For example, if there was bladder endometriosis noticed only during surgery, the chance for removal of the disease from the bladder is missed since this aspect of the surgery was not discussed with the patient prior to the operation. Deep endometriosis involving the ligaments and nerves not tackled during surgery could leave residual pain that continues to affect the patient in a significant way. Scar tissue and adhesions involving the various pelvic organs not picked up and tackled may continue to affect the patient’s potential for fertility.
Hence, a thorough and accurate endometriosis mapping is vital and essential in all aspects of treatment of endometriosis.
Conclusion
The different faces of Endometriosis means that every woman suffering from endometriosis might potentially experience the condition differently — some might be affected less, and others more. Regardless, the impact on one’s quality of life cannot be underestimated.
It is unfortunate that so many women are only seeking care after many years of living with endometriosis, especially when diagnosing and management approaches are advancing with time. As an endometriosis specialist and an advocate for early detection (which was the main reason I started the Endometriosis Awareness Program in Singapore in 2012) , I am excited to be part of these developments and more importantly, committed to helping more women manage their endometriosis and live life like those without the condition.